Back pain is a very common condition. According to the NIH, about 80% percent of adults suffer from lower back pain at some point in their lifetime. It is the greatest cause of work-related disability and one of the top reasons for workplace absences.
The American Chiropractic Association notes that back pain is the second most common reason for visits to the doctor (after respiratory infections) and that half of all working Americans experience back pain symptoms each year.
Back pain can be felt anywhere from the neck down, but the majority of cases are associated with the lower back or lumbar spine. The pain can develop due to problems with the bones, muscles, ligaments, joints, nerves or spinal cord. However, most cases are described as ‘non-specific’, meaning there is no obvious cause.
Back pain tends to last anywhere from a few days to a few weeks. The pain is considered ‘chronic’ if it persists for more than three months.
Usual treatments for acute back pain include over-the-counter analgesics such as ibuprofen, muscle relaxers or prescription painkillers such as codeine.
Severe or chronic back pain may be treated with physical therapy or manual therapy (chiropractic). Surgery is only recommended for specific medical conditions and used as a last resort.
None of the home remedies here will provide instant pain relief. However, they can help to reduce the intensity and frequency of your back pain over time. They can also help to lower your risk of experiencing back pain in the future.
8 Evidence-Based Home Remedies for Back Pain
1. Vitamin D
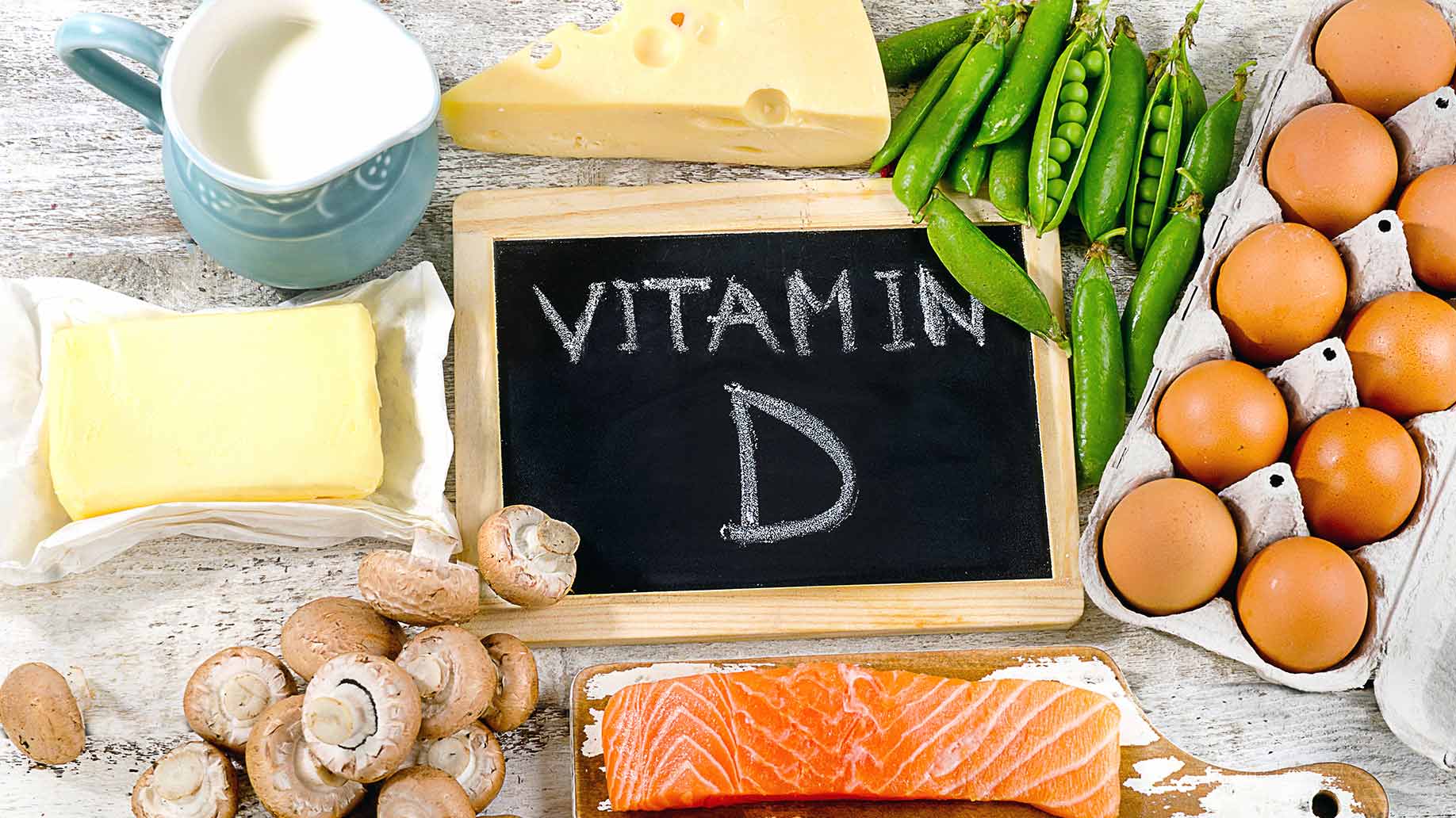
Vitamin D is vital for calcium absorption and building strong bones. A deficiency in vitamin D can lead to the softening of bone surfaces in the spine, weaker muscles in the back and inflammation in the vertebrae.
Research has shown that patients with low back pain have significantly lower blood levels of vitamin D than healthy controls.
A Brazilian study investigated the association between back pain and vitamin D deficiency in 9,305 postmenopausal women. Blood tests showed that 24% of the women had low levels of vitamin D. Questionnaires revealed that they had more back pain than women with normal vitamin D levels, and the pain was more frequent and more severe. The low vitamin D participants also reported more restrictions to daily activities such as putting on socks or getting out of a car.
A clinical trial published in Pain Physician assessed the impact of vitamin D supplementation on 68 patients with chronic lower back pain. All of the participants were deficient in vitamin D and had been experiencing back pain for at least 3 months. They filled out pain and disability questionnaires at intervals throughout the study.
Patients were given high-dose vitamin D supplements for 8 weeks or until blood tests showed that their vitamin D levels were within normal range. They were then given a maintenance dose of vitamin D for 6-months.
Pain scores significantly decreased after 2 months of supplementation. After 6 months, 63% of patients achieved effective pain relief, defined as a 50% or greater reduction in pain scores. Patients also had a significant reduction in functional disability.
Method: While foods such as oily fish, eggs, liver and mushrooms provide some vitamin D, it’s difficult to obtain all you need from your diet.
Your body produces vitamin D in response to UV rays of sunlight. If you live in a sunny climate, try to expose your skin to the sun for at least 15 minutes a day between the hours of 12 pm to 2 pm.
If you live in a climate with cold, dark winters, you may need a daily 10 mcg vitamin D supplement to avoid deficiency. Vitamin D also helps to battle against seasonal anxiety and depression.
Recommended:
- Vitamin D3 5,000 IU – Non-GMO in Cold Pressed Organic Olive Oil
- Vitamin D3 5000 IU Organic Vitamin D, Non-GMO
2. Medium-Firm Mattress
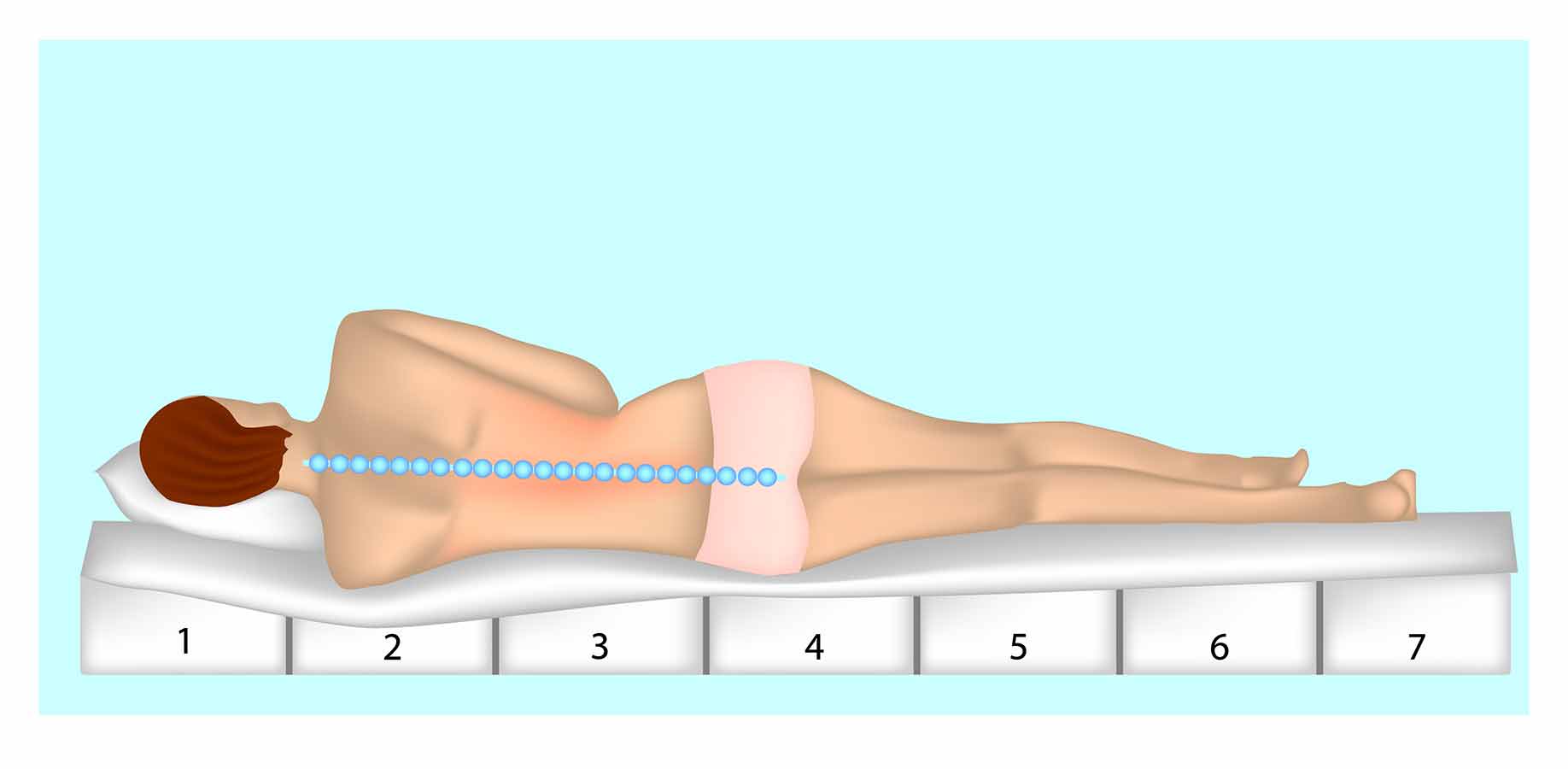
Although extra-firm mattresses are often recommended for people with back pain, a medium-firm mattress may be a better choice.
Research has shown that when a person lies on their side on a hard mattress, only the hip and shoulder are supported and the spine flexes toward the mattress. On a soft mattress, the hip and shoulder sink down and the spine bends away from the mattress. A medium-firm mattress offers the best support for the lower back.
A controlled trial published in The Lancet assessed the effect of mattress firmness on 313 patients with chronic lower back pain. The participants were randomly assigned to sleep on either a firm mattress or a medium firm mattress. They were not told which type of mattress they had received.
After 90 days, the group who slept on the medium-firm mattresses had less pain in bed, less pain on rising and less disability than patients with firm mattresses. Throughout the study, participants with medium-firm mattresses also had less lower back pain during the day and while lying in bed.
A study published in Applied Ergonomics tested the effect of prescribed mattresses on 27 patients diagnosed with lower back pain and stiffness. For 3 weeks, participants slept in their own beds and rated their back and shoulder pain, sleep quality and comfort. The patients’ beds were then replaced with medium-firm mattresses layered with foam and latex. They continued rating their pain and sleep quality for the following 12 weeks.
Back pain and stiffness progressively improved while sleeping on the new mattress and physical discomfort decreased. There was also a significant decrease in the number of ‘poor sleep days’ per week.
In a study published in the Journal of Chiropractic Medicine, 59 men and women kept a record of their back pain and sleep quality for 4-weeks while sleeping in their own beds. They also completed a stress questionnaire. Participants’ beds were then replaced with new medium-firm ones. They rated their back discomfort and sleep quality for a further 4 weeks and repeated the stress questionnaire.
The medium-firm bedding systems reduced back pain by approximately 48% and improved sleep quality by 55%. Symptoms of stress also significantly decreased.
Method: If your mattress is uncomfortably hard or soft and saggy, it may well be contributing to your back pain. While a new medium-firm mattress is an expensive investment, it could be cheaper than repeated visits to a chiropractor.
If you can’t afford a new mattress, look for bargain deals on a memory foam mattress topper. A medium-density foam (60kg/m³) will provide medium-firm support.
Recommended:
3. Fish Oil

Fish oil, rich in omega-3 essential fatty acids, has been shown to reduce pain and inflammation associated with a range of health conditions.
For example, a meta-analysis of 17 randomized, controlled trials found that omega-3 supplementation reduced joint pain and stiffness in patients with rheumatoid arthritis, inflammatory bowel disease and menstrual cramps. Research suggests that the omega-3 found in fish oil could also be an effective treatment for back pain.
A study published in Surgical Neurology investigated the use of fish oil for pain relief. Researchers followed 250 participants that had been evaluated by a neurosurgeon for neck or back pain. Most of the patients had been diagnosed with degenerative disc disease (DDD), and all of them were taking prescription non-steroidal anti-inflammatory drugs (NSAIDs) to control their pain.
For 2 weeks, the participants were given daily fish oil supplements containing 2,400 mg of omega-3 EFAs. Patients were then asked to cut the dosage of omega-3 in half and were given the option to reduce their use of NSAID medications.
After an average of 75 days on fish oil, patients returned questionnaires about spine pain, joint pain and level of NSAID usage. The survey data showed that 60% of patients had an improvement in overall pain and joint pain, and 80% were satisfied with their improvement. As a result, 59% of patients had stopped taking NSAIDs and 88% said they would continue to take fish oil supplements.
More evidence that fish oil can reduce back pain comes from a trial involving 20 patients with asthenopia, the medical term for eye-strain. Asthemopia is often associated with back pain because both conditions are common in people who sit in front of computer screens for hours at a time.
The participants were randomized into 2 groups. The treatment group received a supplement containing fish oil along with bilberry extract and lutein (thought to be effective for maintaining eye health). The other group received a placebo.
Before and after 4 weeks of supplementation, subjects completed a questionnaire about their symptoms. Symptoms such as eye fatigue, eye flicker and eye redness did not improve significantly more in the treatment group than in the placebo group. However, the fish oil supplement did significantly improve symptoms of low back pain and shoulder stiffness.
Method: You can increase the amount of omega-3 in your diet by eating at least 2 portions of oily fish a week. Examples include trout, salmon, fresh tuna, mackerel, herring and sardines.
Alternatively, take a fish oil supplement or an algae-based omega-3 supplement containing DHA and EPA.
Recommended:
- Omega-3 – Organic Fresh Catch Fish Oil
- Wild Alaskan Salmon Oil with Omega-3 + Vitamin D3, Sustainably Caught
4. Yoga

Several aspects of yoga practice can reduce back pain. Holding certain yoga positions strengthens muscles in the back.
Yoga stretches reduce muscle tension and promote flexibility in back muscles and joints. Yoga poses improve posture, align the body, and help to maintain the natural curvature of the spine.
A randomized trial published in the Annals of Internal Medicine compared the effectiveness of yoga and usual care for back pain. Researchers recruited 313 volunteers who had visited a general medical practice with chronic or recurrent low back pain.
Participants were randomized into 2 groups. The intervention group was offered a 3-month program of weekly 75-minute yoga classes. The control group continued with usual care. All participants filled in a standard back pain and disability questionnaire at the beginning and end of the study. The yoga group had significantly greater improvements in back function at 3, 6, and 12 months compared to the usual care group.
A randomized trial compared the effectiveness of yoga and physical therapy for chronic lower back pain. A total of 320 patients being treated for back pain were assigned to 3 groups. One group received yoga classes every week for 3 months, one group had 15 visits to a physical therapist over 3 months, and a third group received self-help educational materials. During the 9-month maintenance phase of the study, patients continued yoga or physical therapy exercises at home.
The yoga and physical therapy groups showed almost the same amount of improvement in pain and physical function at 3 months and one year. Both interventions produced similar improved scores for quality of life. The yoga and physical therapy groups were also about 21% less likely to use pain medication after 3 months compared to the education group. Researchers concluded that yoga was just as beneficial as standard physical therapy for treating lower back pain.
Method: If it’s inconvenient for you to attend a yoga class, you can practice at home. Videos that demonstrate yoga poses for back pain are available online. You can also purchase ‘yoga for back pain’ DVDs. For best results, aim to do at least two 60-minute yoga sessions a week.
Recommended:
- Yoga Therapy for Back Pain and Stress Relief
- Yoga All Purpose Anti-Tear Exercise Yoga Mat with Carrying Strap
5. Sleep

Lack of sleep aggravates back pain in several ways. During sleep, the body releases growth hormones which stimulate muscle repair. Without adequate sleep, strained back muscles don’t have a chance to recover and are less able to support the spine and keep it in aligned.
Research has shown that the spinal discs have an internal 24-hour body clock. Disruptions to circadian rhythms due to irregular or inadequate sleep may contribute to degenerative intervertebral disc disease. In addition, lack of sleep lowers the pain threshold, intensifying the perception of backache.
A study published in Arthritis and Rheumatology investigated the effect of sleep quality and pain intensity in patients with acute lower back pain. Researchers analyzed data from 1,246 patients with recent-onset lower back pain. At the beginning of the study, and for the following 12 weeks, patients recorded their sleep quality on a 4-point scale ranging from ‘very bad’ to ‘very good’. They also rated their back pain on a 10-point scale ranging from ‘no pain’ to ‘worst possible pain’.
Analysis of the data showed that for every one-point decrease in sleep quality, back pain intensity increased by two points. On the 10-point scale, patients with very bad sleep quality rated their pain as 6 points higher than patients with very good sleep quality.
A Finnish study investigated the association between sleep disturbances and lower back pain in 360 working male firefighters. Participants filled in health questionnaires at the beginning of the study that asked them to estimate how many days they had experienced radiating or local lower back pain in the last 12 months. They also filled in a questionnaire about sleep disturbances and daytime fatigue. The men provided additional data after 3 years and at the end of the 13-year study.
The prevalence of radiating lower back pain increased from 16 to 23% during the 3-year follow-up and rose to 29% during the 13-year follow-up. Participants who reported sleep problems at the beginning of the study were almost two and a half times more likely to develop new back pain or to develop chronic radiating back pain.
A study published in the Clinical Journal of Pain examined the bidirectional relationship between back pain and sleep quality. A total of 80 patients with lower back pain completed a sleep diary. A subgroup of 50 patients wore an electronic armband to measure their sleep over the course of a week. All of the participants rated their back-pain intensity twice a day.
The data showed that difficulty falling sleep, waking after sleep onset, or poor quality sleep were all followed by a day with higher back-pain intensity. The researchers detected a vicious cycle. A day with higher back pain scores was associated with a decrease in sleep quality the following night, as well as an increase in time taken to fall asleep and waking up during the night.
Method: Follow these 7 Tips on How to Get Better Sleep.
Recommended:
- All Natural Sound Machine
- Soft Earplugs
- Silk Sleep Mask
- Blackout Pleated Paper Shade
- Plug-in LED Night Light Lamp with Dusk to Dawn Sensor
- Blue Light Blocking Computer Glasses with SCT-Orange Lens
- Wake-Up Light With Colored Sunrise Simulation
6. Sitting Time

Increasing numbers of people in the industrialized world spend most of their working day seated in an office chair. Sitting increases stress on the spine and back muscles.
Research has shown that individuals who are sedentary in an office environment are more prone to back pain than those who move around more. Fortunately, research also suggests a simple solution to reduce lower back pain symptoms: frequent, short, standing rest breaks.
A Danish study investigated the association between sitting time and lower back pain in 201 blue-collar workers. Participants were recruited from 7 occupations with varying amounts of time spent seated. Workers were asked to rate their worst intensity of lower back pain during the past month on a 10-point scale ranging from ‘no pain’ to ‘worst imaginable pain’.
All of the participants were fitted with accelerometers on their thighs and torso which they wore for 4 continuous days. The devices objectively measured sitting time and recorded the data. Analysis showed that high sitting time was positively associated with high lower back pain for occupational sitting time, leisure sitting time and total sitting time.
A study published in Human Factors compared interventions aimed at reducing musculoskeletal discomfort in a sedentary workplace. Four different workstations were installed in a call center: a conventional workstation, a sit-stand workstation, a conventional workstation with software that reminded workers to take a standing break, and a sit-stand workstation with break-reminder software. Worker discomfort was measured by a survey and by video monitoring.
Short-term discomfort in the shoulders, upper back and lower back was significantly reduced when workers were periodically reminded to take a break, independent of workstation type. Productivity increased by about 10%.
Method: If you spend most of the day sitting in front of a computer screen, try to move every 20 minutes. Stand, straighten your back and roll your shoulders.
If you can, set an alarm on your PC or phone to remind you to get up once an hour and walk to the water-cooler, coffee machine or around the office.
Use your breaks to take short outdoor walks rather than eating at your desk or checking email. Take every opportunity to move. If you don’t need to type-in data, stand and pace when talking on the phone.
Recommended:
7. Sitting Posture

One study of office workers found that subjects largely worked in a screen-oriented upright position and rarely reclined in their seats.
While it’s true that slouching over a desk is bad for your spine, constantly sitting up straight can also lead to back pain. A reclining position will shift your weight onto the backrest, allowing back muscles to relax and takes the pressure off spinal discs.
A study presented at the annual meeting of the Radiological Society of North America used whole-body positional MRIs to determine which sitting position put the least biomechanical stress on the lumbar spine. The researchers recruited 22 healthy volunteers with no history of back pain and asked them to assume 3 different sitting positions.
They were scanned slouching forward at about a 70-degree angle, sitting straight upright at a 90-degree angle or reclining backward at a 135-degree angle. Measurements were taken of spinal disk height and movement in each position.
The relaxed, reclining sitting position was shown to cause the least strain on the lumbar spine, most significantly when compared with an upright seating posture.
Method: Experiment with adjusting your office chair so that you naturally lean back slightly rather than sitting up straight or leaning forward. Sit with your feet flat on the floor. Your back should be in contact with, and supported by the chair.
If you need to sit upright to type, adopt a relining position when performing other tasks such as reading reports.
Recommended:
8. Exercise
A general exercise program that improves muscular strength, flexibility and aerobic fitness can help to decrease back pain in several ways:
- Increased core muscular strength supports the lumbar spine.
- Increased flexibility of tendons and ligaments in the back enhances range of motion and functionality.
- Aerobic exercise stimulates the flow of blood and nutrients to soft tissues in the back, accelerating the healing process and reducing stiffness.
- Exercise raises levels of endorphins, the brain’s ‘feel good’ chemicals, providing a natural form of pain relief.
A systematic review published in Healthcare examined the effects of exercise and physical activity on back pain. Researchers complied data from 14 studies of exercise intervention programs for adults with non-specific chronic lower back pain.
They found that all types of exercise studied were beneficial for back pain sufferers including moderate aerobic exercise, muscle strength and core stabilization exercises, and stretching and flexibility exercises such as Pilates.
A randomized controlled trial published in Clinical Rehabilitation compared an aerobic walking program and a muscle strengthening program for 52 sedentary patients with chronic lower back pain. One group performed moderate-intensity treadmill walking. The other group conducted a series of muscle strengthening exercises. Both programs involved 2 sessions a week for 6-weeks.
At the beginning and end of the study, patients conducted a 6-minute walking test and back muscle endurance test. They also filled in questionnaires about back pain and disability.
Both exercise groups significantly improved in all outcome measures. Back pain was reduced by 20% in the aerobic exercise group and 15% in the muscle strengthening group.
Method: The ideal exercise program for back pain involves muscle strengthening exercises, aerobic activity and flexibility exercises. However, most people find it difficult to stick to this type of regime. Since any form of moderate intensity exercise is helpful for back pain, choose a type of physical activity that you enjoy and can fit into your daily routine.
You don’t need to join a gym or a sports team. Around 150 minutes per week of brisk walking, cycling, hiking, swimming or dancing can all be beneficial.
Recommended:
Final Word
Back pain is often preceded by minor discomfort, so listen to your body. Be aware of your posture and avoid positions (such as slouching or twisting) that strain your spine or back muscles.
If you’re sitting and notice your back muscles start to feel tense, stand up and stretch or go for a walk. If you can’t find a comfortable sleeping position, or frequently wake up with a stiff back, consider a new mattress.
Be sure to see your doctor if your back pain is accompanied by other worrying or worsening symptoms. Back pain that occurs along with abdominal pain, numbness in the groin or buttocks, incontinence, or weakness in the legs could be the sign of a serious problem.









I have severe pain along the spinal code please help to know home remedy for me to manage the pain. I have gone to many hospital but no proper relief they just give pain killers.Please help me I am a secretary in a public government office.
thanks.
Visit a reputable Ayurvedic doctor or chiropractor right away. If it is severe, make an appointment with a spine specialist who uses the least invasive approaches first.
Before consulting a doctor of Physiotherapist, we all try some home remedies. Your tips and home remedies both are quiet good and seems effective. Thanks for sharing.
okay
I agreee
Thanks for sharing the valuable tips to overcome lower back pain.
Tha for your inspiring words
Well Tips but I no body follow strictly.
Thanks for this inspiring words from great researchers and am happy to know that what am really pasting through will soon be taken care off (back pain0).
This is a great article, with helpful information. . In addition to the fish oil, and vitamin D, I’d like to mention Turmeric as a wonderful supplement too.
Back pain has been known to steal many people’s joy. If it lingers for long it can indeed affect your mood negatively.
No one wants to go through all day with a lingering pain in their lower back or nay part of their body.
So you did right by publishing this piece.
Is it okay to sleep on the the floor. The floor is made up of hard tiles with a single pillow? How does it affect the spine?